Wellcare Health Plans, Inc., is pleased to announce that we will be able to receive Electronic Attachments (ANSI ASC x12, 275 transactions) through our preferred clearinghouse, Change Healthcare. Providers may submit unsolicited attachments (related to pre-adjudicated claims). In addition, the Plan may solicit claims attachments via 275 transactions through the clearinghouse to the billers that use Change Healthcare. At this time, Electronic Attachments (275 transactions) are not intended to be used for appeals, disputes or grievances.
What are Acceptable Electronic Data Interchange Healthcare Claim Attachment 275 Transactions
Electronic Attachments (275 transactions) are supplemental documents providing additional patient medical information to the payer that cannot be accommodated within the ANSI ASC X12, 837 claim format. Common attachments are certificates of medical necessity (CMNs), discharge summaries and operative reports to support a Healthcare claim adjudication. Again, the 275 transaction is not intended to initiate provider or member appeals, grievances or payment disputes. Please use the Quick Reference Guide for correct mailing addresses or phone numbers for appeals, grievance, authorization or payment disputes. Go to www.wellcare.com and select the ‘State’ and ’Product’. Then from the tool bar, select ‘Provider’ and from the drop down arrow select ‘Overview’. Scroll to find and click on that State/Product Quick Reference Guide.
Why submit a Healthcare Claim Attachment 275 Transaction?
Sending necessary attachments electronically offers a faster, more streamlined and cost-efficient process over printing and mailing a paper attachment on a paper submission.
When to submit a Healthcare Claim Attachment 275 Transaction?
When supporting document is required to support or substantiate claim adjudication (Invoices, Medical or Utilization review notes or if requested by Wellcare). The Plan uses the ANSI ASC x12, 277R transaction Health Care Claim Request for Additional Information to transmit the request. The provider uses the Electronic Attachment 275 transaction to respond.
How to submit a Healthcare Claim Attachment 275 Transaction?
- A separate Transaction Set Header/Trailer (ST/SE) must be sent for each claim response.
- The EDI 275 can accommodate multiple responses for a specific claim. (See the LX segment section for additional details).
- Providers can send unsolicited 275 attachment within a Fee For Service (FFS) 837I or 837P transaction set or they may send the 275 transaction separate of the 837 transaction. When sending separately, WellCare suggests you transmit them on the same day.
- The Plan will attempt to match the 275 transaction to a claim or member. If a match is not found, the Plan will send a notification that reads, “We have received your 275 electronic attachment, but the information submitted does not match to a claim or authorization request on file.”
Definitions:
- Solicited 275 Transaction: Provider receives a 277R response from the payer, requesting additional information. Provider submits a 275.
- Unsolicited 275 Transaction: Provider submits supplemental information on a pre-adjudicated claim submission that is not required on the actual submission but will assist the payer in determining accurate benefits during the adjudication process. Matching Logic between 837.
Please share the below section with your technical support team.
The Plan is expecting the following data alignment in order to execute match logic.
|
Solicited 277R to Attachment (275) Match Logic |
||||
|
277R Transaction |
Action |
275 Transaction |
||
|
Element Name |
Loop/Segment |
Element Name |
Loop/Segment |
|
|
Payer Claim Control Number |
Loop 2200D TRN02 |
Compare to |
Payer Claim Control Number |
Loop 2000A TRN02 |
|
Unsolicited 837 to Attachment (275) Match Logic |
||||
|
837 Transaction |
Action |
275 Transaction |
||
|
Element Name |
Loop/Segment |
Element Name |
Loop/Segment |
|
|
Attachment Control Number |
Loop 2300 PWK06 |
Compare to |
Attachment Control Number |
Loop 2000A TRN02 |
|
Billing Provider NPI |
Loop 2010AA NM109 |
Compare to |
Billing Provider NPI |
Loop 1000C NM109 |
|
Subscriber ID |
Loop 2010BA NM109 |
Compare to |
Subscriber ID |
Loop 1000D NM109 |
|
Patient Name |
If loop 2010CA is included, then 2010CA NM103 and NM104, else 2010BA NM103 and NM104 |
Compare to |
Patient Name |
Loop 1000D NM103 and NM104 |
BIN Segment Formatting Rules
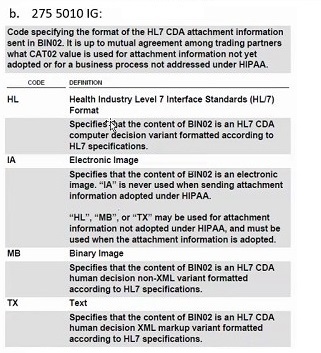
The code transmitted in the CAT02 element details the formatting of the attachment contained in the BIN segment. If you are using HL, TX or MB, please note you must be using a HL7 CDA XML Version 2 or greater to avoid a rejection for not being able to convert the data to a readable file type. Below are the four codes accepted in the CAT02 element:
BIN Segment Formatting Rules
The below rules for each format must be followed to ensure the attachment can be processed and used by the Plan.
- CAT02 = HL —attachment contains only XML, including an HL7 CDA header and body. The entire attachment is encoded in hexadecimal.
- CAT02 = TX — attachment contains only XML, including an HL7 CDA header and body. The entire attachment is encoded in hexadecimal
- CAT02 = MB —attachment contains an XML HL7 CDA header and a non- XML body. The non XML body is BASE64 encoded; the entire attachment is then encoded in hexadecimal. The non XML body must contain of one of the following file types:
- MSWORD
- Excel
- GIF Image
- TIF Image
- JPEG Image
- PNG Image
- Text (Plain, RTF or HTML>
- CAT02 = IA —attachment contains only a MIME header and BASE64 encoded file. The entire attachment is then encoded in hexadecimal. Like the MB, the encoded file must be only one of the following file types:
- MSWORD
- Excel
- GIF Image
- TIF Image
- JPEG Image
- PNG Image
- Text (Plain, RTF or HTML)
Resources:
www.wpc-edi.com
Additional Information to Support a Health Care Claim or Encounter (275) - ASC x12N/005010X10 Based on Version 5, Release 1 February 2008 ASC X12 Standards for Electronic Data Interchange Technical Report Type 3.
www.HL7.org This is an ANSI Accredited Standards Development Organization (SDO) whose domain is clinical and administrative data. See section 1.7.4 for additional details.
For questions about this communication or more assistance with 275 Claim Attachment Transactions, please contact our EDI team at EDI-Master@wellcare.com.
For all other inquiries for claim status, authorization or eligibility, please contact Provider Service by going to Wellcare website and selecting the correct State. Then click on “Contact Us” to find the correct provider’s service phone number for the member’s plan.